When we consider how complex the human brain is, the tissue surrounding our control systems can seem pretty insignificant in comparison.
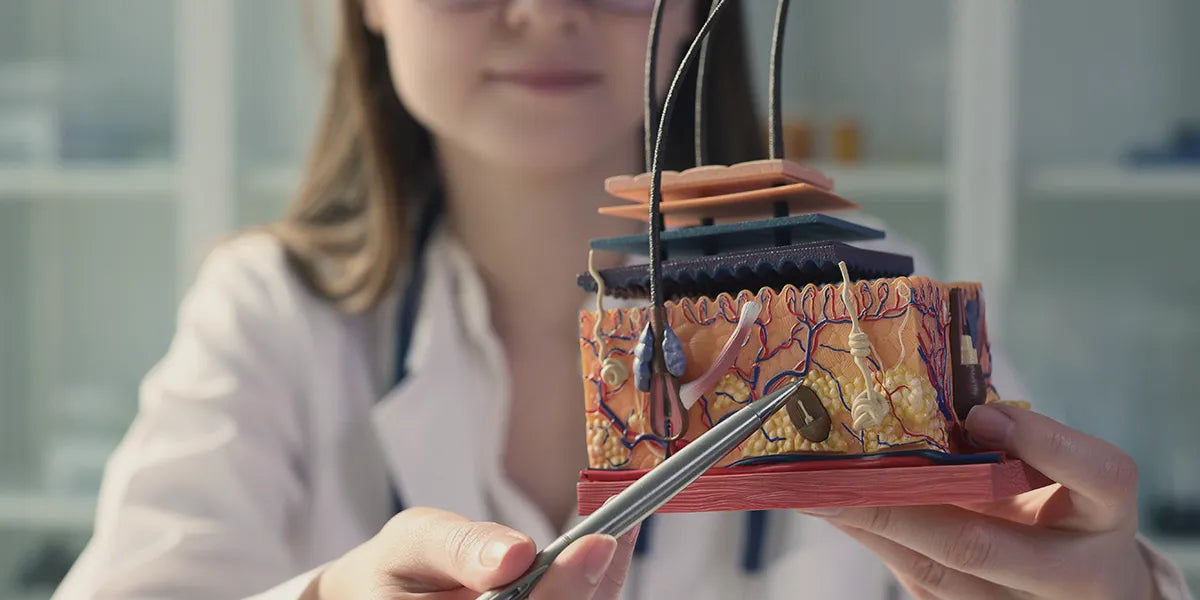
But in reality, scalp anatomy is rather sophisticated in its own right. The scalp contains 5 distinctive layers that vary in function, form and cellular composition. These delicate membranes and connective fibers contain an intricate network of blood vessels, nerves and hair follicles, among other things. All of this is housed within 5-10 mm of tissue surrounding your skull and central processing system (Ungar et al. 2018).
XYON's SiloxysSystem™ Gel technology helps make sure your medication goes where it's needed and not where it's not.


Target hair loss and minimize side effects with SiloxysSystem™ Gel.
Topical medications for male pattern baldness can effectively target hair loss once they have penetrated the outermost layer of scalp skin. Beyond this, drugs like finasteride and dutasteride are more likely to enter the circulatory system through blood vessels found in deeper tissue. This increases the likelihood of widespread systemic absorption, typically associated with a greater risk of sexual and other side effects.
In this article, we get acquainted with the anatomy of the scalp and shed light on how different topical formulations interact with the layers within it. Keep reading for an up-close and personal look at your scalp.
The scalp skin
The outermost covering of your scalp, the skin surrounding your cranium typically measures between 3.5-5.5 mm. In addition to acting as a physical barrier, the skin of the scalp has several other functions including temperature regulation, hormone production, UV light filtration and moisture regulation (Yousef et al. 2021).
The scalp skin contains 2 distinct layers, each made up of several different cellular membranes: the epidermis and the dermis.
The epidermis
The epidermis acts as a protective barrier to an expansive network of blood vessels, tissue, nerves and bone beneath. While the thickness of this layer varies at different points across the body, it is only about 1.5mm thick at the scalp.
This level of scalp skin contains 5 distinct cellular layers: the stratum corneum, the stratum lucidum, the stratum granulosum, the stratum spinosum and the stratum basale (NIH).
The stratum corneum is the outermost cellular level, spanning the surface of the skin. It’s made up of cells called keratinocytes, the same type of cells that form the hair shaft (Martel et al. 2021). The stratum basale is the innermost membrane within the epidermis. It separates the more central cellular levels from the dermis beneath.
The dermis
The dermis is the thicker of the two layers of skin, typically measuring between 2-4mm (NIH). While it contains fewer distinct layers, it houses more functional elements than the epidermis. Among these are various glands, nerves, connective tissue, blood vessels and hair follicles.
Dihydrotestosterone (DHT), the androgen associated with AGA, is also produced within this specific layer of skin.
The dermis can be separated into two general levels, each housing different components: the papillary dermis and reticular dermis.
The papillary dermis lies directly beneath the epidermis. It contains sweat, sebaceous and endocrine glands, as well as a complex network of small blood vessels called capillaries that supply oxygenated blood to the scalp skin and hair follicles.
The reticular dermis is the more visceral dermal layer, found alongside the hypodermis. It’s made up of mostly collagen and elastin. These two cell types lend themselves to skin elasticity and make this layer more dense than the papillary dermis (Brown and Krishnamurthy 2021).
Normally, healthy terminal hairs sprout from follicles rooted in this deeper dermal layer, extending into the subcutaneous tissue beneath.
Dense connective tissue
The connective tissue layer is made up of lipids (fat molecules) and fibers bound together in one membrane. It’s attached to both levels of the scalp skin and all three move as one unit (Germann et al. 2021).
Also called subcutaneous fat, (sub-under, cutaneous-skin) this protective layer insulates the skull. The thickness of the lipid layer varies at different points on the body and differs in relation to body fat percentage, to a degree. Its function remains the same, regardless of thickness: subcutaneous fat buffers external force and protects bone, tissue and important functional components within these deeper layers.
Blood vessels
The subcutaneous connective tissue contains a higher density of blood vessels than the dermis, which aids in hair growth. Healthy hair follicles that extend into this layer receive nutrients from arteries carrying oxygenated blood away from the heart, allowing terminal hairs to become longer and reach maturity.
Several major inbound arteries carrying oxygenated, nutrient-rich blood to the scalp are found within the dense connective tissue layer (Germann et al. 2021):
- The internal and external carotid arteries
- The posterior intercostal arteries
- The subclavian artery
The superficial temporal vein is one major outbound blood vessel found within this layer. This vein circulates blood from the scalp back towards the heart, travelling through a network of smaller blood vessels within the more peripheral loose areolar connective tissue layer beneath the aponeurosis.
Other noteworthy veins that move blood away from the scalp include:
- The supratrochlear vein
- The supraorbital vein
- The occipital vein
- The posterior auricular vein
Lymphatic Drainage
The dense connective tissue layer also contains lymphatic vessels that maintain immune function within the scalp. The parotid, cervical, submandibular, occipital and mastoid lymph nodes are found within this level, circulating cellular fluids containing lipids, immune cells and cellular waste away from the scalp (Tajran and Gosman 2021).
Aponeurosis (galea aponeurotica)
The scalp doesn’t contain a layer of muscle tissue; it’s “all brain, no brawn”. The epicranial aponeurosis (or just aponeurosis) is an intermediate connective membrane that exists in place of striated muscle tissue. This dense sheath is sandwiched between the subcutaneous (sub- under, cutaneous- skin) connective tissue and the loose areolar connective tissue beyond.
Primarily composed of the protein collagen, the aponeurosis is loosely striated and visibly fibrous. Similar to ligaments and tendons found throughout the body, its structure borders elasticity and total rigidity. There are no blood vessels or nerves embedded within the connective tissue layer; absorption cannot occur within this level of tissue at the scalp.
From a functional standpoint, there is no need for a high degree of mobility at the crown of the head. The aponeurosis acts as a passive structural element, holding layers above and below it together. This membranous layer generally follows the shape of your natural hairline, extending across the crown of the head and connecting several craniofacial muscles that exist apart from the scalp (Tajran and Gosman 2021).
A series of three muscles found just above the ears:
- Superior auricular muscle
- Anterior auricular muscle
- Posterior auricular muscle
Both regions of the occipitofrontalis muscle:
- The frontalis (located at the front of the head, spanning the forehead)
- The occipital (found at the nape of the neck, extending across the base of the head)
Loose areolar connective tissue
The loose areolar connective tissue connects the aponeurosis to the pericranium beneath it. This layer is more fluid than both the dense connective tissue layer and the aponeurosis, allowing for lateral movement in response to traction and shifting between the layers above and below.
Venous drainage
This loose tissue layer contains a complex network of tiny emissary veins. These circulatory pathways connect the dense connective tissue layer to complex clusters of blood vessels deep within the skull, called venous sinuses. Deoxygenated blood is distributed to different venous sinuses via emissary veins. This 'used' blood is then circulated throughout the body, and eventually makes its way back to the heart (Germann et al. 2021).
The loose areolar tissue layer is often referred to as the ‘danger zone’ of the scalp. Blood vessels embedded within this level of the scalp are typically smaller than those found within more superficial layers.
Bacterial infections, topical medications and any other foreign substances that enter the bloodstream via the loose areolar connective tissue layer are more likely to pose a serious threat to brain health and the body's overall function.
Pericranium
The pericranium is a type of periosteal tissue. This same kind of thin membrane encases all of the bones in your body (Dwek 2010).
The pericranium contains blood vessels that support cell synthesis within the scalp. It consists of 2 layers:
- The outer fibrous layer, which contains fibroblasts that manufacture collagen and other cellular structural elements
- The inner cambium layer, which contains cells that aid in the development of bone tissue
The pericranium is the final layer of tissue before you reach the bone of the skull.
Targeting hair loss with topical drugs
Elevated DHT concentrations at the scalp can negatively impact sebaceous and sweat glands, hair follicle health and normal hair growth. Increased scalp DHT is a leading cause of hair loss in men. It causes the hair growth cycle to be terminated prematurely.
Hair follicles can become miniaturized as a result of elevated DHT within the scalp. These damaged follicles typically produce shorter vellus hairs anchored in the more superficial papillary dermis. Hairs embedded in this dermal layer don’t extend far enough into body to really benefit from nutrient-rich, oxygenated blood transported by blood vessels in deeper tissue layers.
Recall: DHT is produced within the dermis, the deeper layer of the scalp skin. Topical drugs like finasteride and dutasteride have to reach the dermis to effectively target hair loss.
But permeation past this second layer of the skin is not necessary. Transported further away from the scalp and towards the bloodstream, these drugs can negatively impact DHT levels throughout the body.
Once they have entered systemic circulation via blood vessels within the scalp, finasteride and dutasteride carry a greater potential risk of side effects including sexual dysfunction and a lower sex drive.
Scalp anatomy: Takeaway
Choosing a topical medicine to treat your hair loss becomes easier when you understand scalp anatomy. Taking time to consider how medications like topical finasteride interact with each of the scalp’s layers is an important part of your hair growth journey that can help inform your decision.